Recent Research
To address concerns about the impact of specialty hospitals, three federal agencies recently conducted studies: the Government Accountability Office (GAO), an agency that studies federal programs and expenditures on behalf of Congress; the Medicare Payment Advisory Commission (MedPAC), an agency that advises Congress on issues affecting the Medicare program; and CMS (the CMS study was conducted with RTI International, a North Carolina-based research firm). Researchers from the University of Iowa College of Medicine and Georgetown University have also recently published relevant studies.
The following summary discusses what the recent research reveals about the characteristics of specialty hospitals, the patients they treat, their finances and their quality of care.
Hospital Characteristics
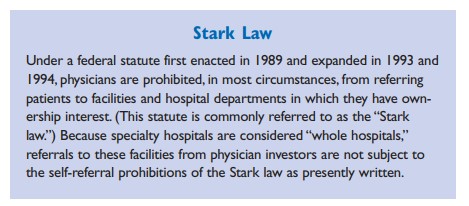
Although single-specialty physician owned hospitals are often categorized generally as “specialty hospitals,” both GAO and CMS identified key differences between types of specialty hospitals. Cardiac hospitals, for example, more closely resemble full service general hospitals than orthopedic and surgical hospitals, which are more like ambulatory surgery centers. Cardiac hospitals, however, are still smaller, more likely to be physician-owned and less likely to have emergency departments than general hospitals. GAO also found that specialty hospitals— regardless of their focus—are more likely than general hospitals to be organized on a for-profit basis.
Patient Selection
The CMS study found that physician ownership has some influence in directing patients to specialty hospitals, but it is not substantial. In contrast, the Georgetown study, which focused only on cardiac hospitals, found that physician owners treat significantly higher volumes of well-insured patients at their own facilities.
The research buttresses a key criticism of specialty hospitals—that they treat a healthier patient population than general hospitals. All of the studies found that patients treated in specialty hospitals are less severely ill than patients treated in general hospitals. Even among patients with the same diagnoses, those treated in specialty hospitals are less likely to have secondary illnesses and complications.
Some members of Congress have recently expressed concerns that specialty hospitals serve a significantly smaller share of ethnic and racial minority Medicare patients than community hospitals. These Congressmen have requested a CMS investigation.
Financial Performance
MedPAC found that the less severely ill patients treated at specialty hospitals tend to be more profitable than the patients treated at general hospitals. These patients are more profitable because Medicare pays a set amount for a patient with a particular diagnosis, but some may have fewer complications and require fewer days in the hospital and less intensive treatment. Specialty hospitals also focus on the treatment of patients with specific diagnoses, many of which are more profitable than the broader range of patients treated in general hospitals. As a result of these findings, it is commonly believed that specialty hospitals have a negative financial impact on general hospitals. However, the available research does not demonstrate that specialty hospitals have done measurable financial harm to the general hospitals with which they compete.
MedPAC and CMS both found that specialty hospitals serve a lower proportion of Medicaid patients and provide less uncompensated care than general hospitals, supporting the contention that they limit their services to a more affluent, well-insured population. However, CMS also pointed out that because for-profit facilities pay taxes, from which not-for-profit hospitals are exempt, the “net community benefit,” measured as the sum of uncompensated care and tax payments as a proportion of net revenue, is higher in specialty hospitals than in general hospitals. CMS did not attempt to quantify the value of other community services provided by general hospitals that may not be offered by specialty hospitals.
MedPAC concluded that much of the financial benefit experienced by specialty hospitals is due to specific factors within the Medicare payment system. In response to this finding, CMS recently made revisions to Medicare payment rules that better delineate differences in severity of illness in several categories of patients frequently treated in specialty hospitals. These changes, which took effect on Oct. 1, 2005, decrease payments for some cases and increase payments for others. The overall impact of these changes on referral patterns and hospital finances remains to be seen.
Additional changes to Medicare payments to better adjust for severity of illness and more accurately reflect the actual costs of providing care are still under development.
Quality of Care
The CMS and University of Iowa studies examined quality of care and patient outcomes at cardiac and general hospitals. The researchers focused only on cardiac specialty hospitals because of their high inpatient utilization compared to orthopedic and surgical hospitals. The studies found no significant differences in mortality rates between specialty and general hospitals after adjusting for patient characteristics and procedural volume. One set of adjustments was intended to ensure that severity of illness and other patient factors did not influence the results. Similarly, because there have been claims that there are advantages to specialization above and beyond the “volume effect,” in which better outcomes are related to higher procedural volumes, the researchers adjusted for volume to standardize the analysis.
CMS also found high levels of patient satisfaction with the services and amenities at specialty hospitals.
Next Steps
It is clear that patients treated in specialty hospitals are not as sick as those treated at general hospitals, and there is some evidence that referral patterns are influenced by physician ownership of cardiac hospitals. Less clear, however, is the financial impact of specialty hospitals on general hospitals and the services they provide. In addition, much of the existing research focuses only on the Medicare population, and none directly assesses the effects of the relatively heavy concentration of specialty hospitals in Kansas. To obtain a clearer picture of what is happening in Kansas, KHI and KDHE are analyzing the evolving impact of specialty hospitals on Kansas communities. This analysis will examine what happens to general hospital utilization, profit margins and services when specialty hospitals enter the market.